On December 6th at 8 AM, Dr. Carreira will be at Piedmont Hospital in Atlanta, Georgia presenting on the evaluation and treatment of patients with hip pain in the primary care setting. Hip pain burdens a significant proportion of the population at one time or another, and locating the source of pain in and/or around the hip is often not straightforward. Whether it be a muscle strain, fracture, sprain, joint injury, or arthritis, there are a number of questions that can be asked, physical exam tests that can be performed, and imaging features that can be analyzed, all of which Dr. Carreira will review at Piedmont Hospital to better equip the primary care physician to effectively coordinate care for patients dealing with hip pain.
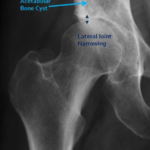
Age can be a narrowing factor in diagnosing patients presenting with hip pain. Older patients (generally ≥50 years old) with limited range of motion and deep aching and stiffness sound the alarm bells for arthritis as the underlying pain generator. X-rays are often diagnostic for arthritis, with the arthritic hip showing some combination of joint space narrowing, thickening (sclerosis) of the hip joint bones, bony overgrowth (osteophytes), and bone cysts (Figures 1,2). Arthritic hips are graded on the severity of the degeneration at the joint using the Tönnis grade classification system which spans from grade 0 through grade 3. This classification system is important in making decisions for patient care, as recent studies have shown that patients with Tönnis grade 2 and Tönnis grade arthritis are more likely to do poorly after hip arthroscopy.1-3
One of the challenges in treating patients with hip pain is determining whether the pain is coming from the joint or from the muscles, tendons, and bony structures of the spine and pelvis outside of the joint. The lumbar spine can be a generator of pain, and pain around the hip can be inappropriately attributed to the hip when the spine is the underlying cause. Patients with a history of low back pain, pain that radiates down the leg past the knee, and symptoms of numbness, tingling, and burning are likely having pain related to the lumbar spine. The flexion, adduction, and internal rotation (FADIR) test, the flexion, abduction, and external rotation (FABER) test, and the “log roll” test are very sensitive for picking up problems related to the hip joint, but these tests are not necessarily specific (Figures 3-5). In other words, when a patient feels pain from these maneuvers during the physical exam, this suggests that a patient’s pain can very well be coming from the hip joint, but other structures around the hip cannot be automatically ruled out as the underlying cause.
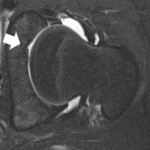
The labrum is a soft tissue that lines the joint and helps reduce the contact forces between the ball and the socket. A torn labrum can be a source of pain and warrant arthroscopic surgical repair. In the cases in which soft tissue injury of the hip joint is suspected, an MRI is very useful for diagnosing these tears (Figure 6). Traditionally, an injection of dye into the joint has been required to determine if the labrum is torn. However, with advances in MRIs, there are higher strength machines (3 Tesla) which are able to effectively pick up labral tearing without requiring an injection prior to imaging.4 Patients with symptomatic labral tearing often (87% of the time!) have some sort of underlying structural abnormality of the bones of the ball and socket.5 Namely, these patients may have some overgrowth of the bone of the socket, a misshapen head of the femur, or quite commonly, both. This abnormal alignment of bone is known as femoroacetabular impingement, or “FAI” for short. These bony abnormalities can be visualized on plain x-rays (Figures 7, 8), MRI, or CT scan. A patient with symptomatic femoroacetabular impingement and labral tearing may be a candidate for arthroscopic surgery, given that no signs of arthritis are present. Patients who are “borderline dysplastic” can also be identified as such with plain x-rays. These patients may be candidates for arthroscopic surgery, as current research on this population is promising at 2-years after arthroscopy.6-8
Patients with hip joint injuries may be treated with conservative measures, which are outlined here:
-
- NSAIDs (naproxen, ibuprofen, motrin, celebrex, etc..): Short courses of these non-steroidal anti-inflammatories are recommended. Please take with food, and consider taking a medicine to protect the gastrointestinal system. This medication should be checked with your primary care physician to make sure that there are no other medical problems that may prevent you from safely taking an NSAID.
- Activity modification: If it is painful to do a certain activity, try to limit this activity until the pain has improved, and then resume gradually. It may be helpful and acceptable to you to avoid impact activities like running, jumping and contact sports. Pool therapy is a great way to offload weight on the joints while maintaining a cardiovascular workout.
- Weight Loss: Extra weight placed on your joints leads to extra stress on these areas. Weight loss may lessen your pain.
- Glucosamine/Chondroitin: This over-the-counter supplement is controversial for joint health. Some studies have shown benefits related to joints and joint disease. This can be found at any local pharmacy like Publix, Target, and Costco. Rare side effects include GI irritation.
- Turmeric: In recent years there has been increased interested in natural supplements that decrease inflammation. Turmeric has limited scientific evidence to supports its benefits.
- Injections (Steroids or Hyaluronic acid): The injection into your joint is to help decrease inflammation and pain. This rarely provides long-term relief and length of relief varies. Other investigational treatments include platelet rich plasma (PRP) and stem cells.
- Surgery: If all else fails, surgery may be performed arthroscopically (through small portal incisions) or open. The type of surgery depends on the location, extent of injury, and any associated abnormalities.
When there is a generator of pain outside of the joint, muscle strains, bursitis and snapping hip are common diagnoses. Trochanteric, psoas, and ischial bursitis as well as tendinopathies of the iliopsoas and gluteal tendons often occur in combination with joint injury. It is important to consider the possibility of a secondary joint injury and thus diagnostic imaging in these patients. The most commonly strained muscle groups are the adductors, rectus femoris, the iliopsoas, and the hamstring muscles. Conservative treatment is appropriate for the vast majority of these strains, with rest, nonsteroidal anti-inflammatories, physical therapy, and corticosteroid injections viable options to manage pain and facilitate recovery. The exception to this rule is with high grade or complete proximal hamstring tears. Surgery is recommended in patients with multiple tendon tearing, especially in patients hoping to return to a high level of activity. Also, patients with chronic pain at the hamstring origin, also known as the SITS bone (ischial tuberosity), and who have significant degeneration and partial tearing at the hamstring origin may be candidates for surgical treatment.9-11
Dr. Carreira looks forward to sharing some of these pearls of wisdom at Piedmont Hospital next month as part of a greater effort to improve quality of care for hip patients seeking relief and efficient and accurate diagnoses.
References
- Skendzel JG, Philippon MJ, Briggs KK, Goljan P. The effect of joint space on midterm outcomes after arthroscopic hip surgery for femoroacetabular impingement. Am J Sports Med 2014;42(5):1127-1133.
- Philippon MJ, Briggs KK, Carlisle JC, Patterson DC. Joint space predicts THA after hip arthroscopy in patients 50 years and older. Clin Orthop Relat Res 2013;471(8):2492-2496.
- Chandrasekaran et al. Outcomes of hip arthroscopy in patients with Tönnis grade-2 osteoarthritis at mean 2-year follow-up: evaluation using a matched-pair analysis with Tönnis grade-0 and grade-1 cohorts. J Bone Joint Surg 2016;98(12):973-982.
- Magee, T. Comparison of 3.0-T MR vs. 3.0-T MR arthrography of the hip for detection of acetabular labral tears and chondral defects in the same patient population. Br J Radiol 2015;88(1053):20140817.
- Wenger DE, Kendell KR, Miner MR, Trousdale RT. Acetabular labral tears rarely occur in the absence of bony abnormalities. Clin Orthop Relat Res 2004;(426):145-150.
- Nawabi DH et al. Outcomes after arthroscopic treatment of femoroacetabular impingement for patients with borderline hip dysplasia. Am J Sports Med 2016;44(4):1017-1023.
- Domb BG et al. Arthroscopic capsular plication and labral preservation in borderline hip dysplasia: two year clinical outcomes of a surgical approach to a challenging problem. Am J Sports Med 2013;41(11):2591-2598.
- Cvetanovich et al. Do patients with borderline dysplasia have inferior outcomes after hip arthroscopic surgery for femoroacetabular impingement compared with patients with normal acetabular overcoverage? Am J Sports Med 2017;45(9):2116-2124.
- Rust DA et al. Functional outcomes and return to sports after acute repair, chronic repair, and allograft reconstruction for proximal hamstring ruptures. Am J Sports Med 2014;42(6):1377-1383.
- Cohen S, Bradley J. Acute proximal hamstring rupture. J Am Acad Orthop Surg 2007;15(6):350-355.
- Domb BG et al. Endoscopic repair of proximal hamstring avulsion. Arthrosc Tech 2013. 2(1):e35-339.