When nonoperative treatments for ankle arthritis fail, the surgical option of ankle arthrodesis (fusion) may be recommendable. The surgery eliminates the painful joint and locks it in place, affecting the up and down movement of the foot, eliminating about 75% of it. The amount of loss of motion from the surgery depends on how much motion has been lost due to the arthritis itself. The side to side movement (inversion and eversion) of the back of the foot is not affected by an ankle arthrodesis. Screws are inserted into the ankle joint to hold the joint together while the fusion occurs. Once the joint is fused the screws are not necessary, but are typically not removed, unless they cause any pain.
Office Appointments and Telemedicine with Dr. Carreira

You can also book an office appointment or a telemedicine visit by calling Dr. Carreira’s office at 404-355-0743. Book now.
General Recovery Facts about Ankle Arthritis
- You will not be walking on the leg for a minimum of 6 to 8 weeks
- In order to stay off your foot, you will need to use crutches, a walker, a wheelchair or a roll about.
- There will be a bulky splint applied to the leg for two weeks after surgery
- Your first follow up visit will be at approximately two weeks to remove the stitches, and a cast will be applied at that time
- If the surgery is on your left ankle, you should be able to drive an automatic vehicle at approximately two weeks.
- You may begin to walk in the cast at about 6-8 weeks, depending upon the extent of bone healing noted on x-rays. Progression in terms of weight-bearing is dependent on your level of comfort also.
- There will be swelling of the foot and ankle for several months
- You will continue to improve your strength for approximately one year after the surgery
Post Operative Recovery
Day 1
- Foot wrapped in bulky splint
- Ice, elevate, take pain medication, and expect numbness in the foot for 12- 24 hours
- Bloody drainage through bandage expected, but do not change the bandage. You can reinforce the bandage with additional dressings.
Days 3-5
- First follow up in the office, the dressing is changed
- Short leg cast is placed
- No weight bearing at all for a minimum of 6 weeks
Weeks 2-3
- Sutures are removed
- Short leg cast is replaced
Weeks 6-8
- Cast removed, X-rays taken
- Another cast may be applied depending on the amount of bone healing noted
Treatment of Joint Arthritis
Dr. Carreira has prepared an information sheet that details the treatment of joint arthritis.
Download Treatment of Joint Arthritis » (PDF: 294KB)
Photos of Ankle Arthritis
A Minimally Invasive Option for the Arthritic Ankle
Arthroscopic Ankle Arthrodesis Has Its Advantages
– An article by Dominic Carreira, M.D. and Brendan Emmons, B.S.
The treatment of ankle arthritis, defined as diffuse articular cartilage loss of the ankle, continues to evolve. Ankle arthrodesis remains a popular choice among patients and surgeons, despite the increased utilization and improved results recently reported with ankle replacement and distraction arthroplasty. A successful ankle arthrodesis that achieves a bony union in good position is often a permanent solution for ankle pain.
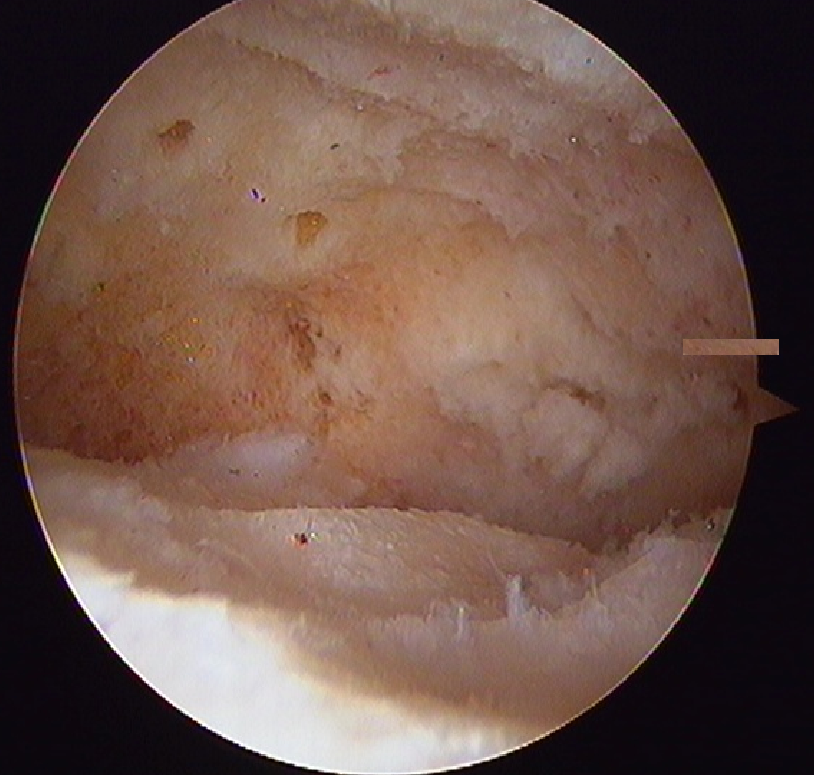
Figure 1. The tibia (above) and the talus (below) after removal of hyaline cartilage and before subsequent fusion. The perforated subchondral bone can be visualized here.
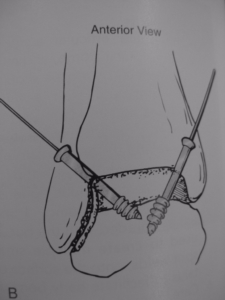
Technically, ankle fusion surgery consists of the following three steps that must be performed effectively to achieve good results: joint preparation, positioning, and compression and fixation. Joint preparation is critical and involves removal of articular cartilage and penetration of the subchondral bone of the joint to expose healthy cancellous bone (Fig. 1). The joint must then be positioned appropriately, and coronal and axial deformities should be corrected. After appropriate positioning, the joint is compressed with orthopaedic implants.

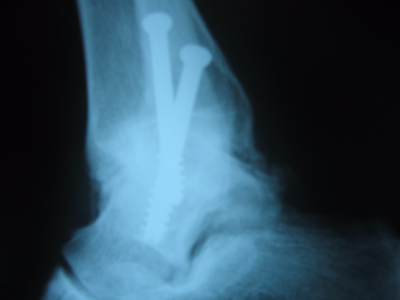
Figure 2. Preoperative AP radiograph demonstrating significant arthritic changes at the tibiotalar joint. This 56-year-old patient’s arthritis had a traumatic etiology.
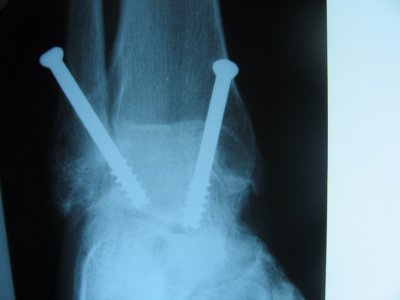
As equipment has evolved, preparation of the joint surface by arthroscopic means has become increasingly popular. Termed “arthroscopic ankle fusion”, the procedure entails the use of arthroscopic shavers and burs to remove the joint surfaces, and drills, picks, curettes and chisels to perforate the subchondral bone. Fixation and compression are usually achieved percutaneously with cannulated screws, resulting in a minimally invasive procedure (Fig. 2 and 3).

Figure 3. Three-month postoperative AP radiograph demonstrating evidence of bony union. Two screws were placed in parallel from the medial side at the time of surgery.
The first description of the technique is credited to Schneider who presented a video of the procedure in 1983. Surgeons who use the arthroscopic technique routinely cite less blood loss, smaller incisions, and a lower infection rate. The overall maintenance of the soft tissue envelope also should be considered as an advantage of the arthroscopic approach, particularly when the possibility of future conversion to arthroplasty exists. The arthroscopic approach may also be useful in cases of soft-tissue compromise or less than ideal protoplasm, such as in elderly patients and in patients with inflammatory arthritis, peripheral vascular disease, venous stasis, smoking history, or diabetes.
What the Literature Shows
A multicenter comparative case series found that arthroscopic ankle arthrodesis patients had shorter hospital stays and improved outcome scores at one and two years when compared to patients who underwent open arthrodesis. Similarly, a retrospective review of open and arthroscopic ankle fusions found significant decreases in time to union and rate of complication in the arthroscopic group. Yet another study reported diminished time of stay and accelerated time to bony union for patients who underwent arthroscopic rather than open arthrodesis.
The most recent systematic review comparing open and arthroscopic approaches concludes that the arthroscopic approach is associated with fewer complications, shorter hospital stays, diminished blood loss, and better outcome scores. Nevertheless, open ankle arthrodesis is more commonly performed.
Cost differences between the two approaches are worth noting. A 2010 retrospective cost analysis comparing outpatient arthroscopic procedures with inpatient open procedures found that arthroscopic procedures resulted in significantly lower total site charges and lower expenses for third-party payers. Despite these advantages, the arthroscopic approach does have contraindications and associated complications. A relative contraindication to arthroscopic surgery is large bone defects, such as significant (> 15 degrees) deformities and large osteophytes. In these situations, the open approach may offer improved visualization and access to the joint, permitting the surgeon to correct these larger deformities.
Arthroscopic fusion has also been unsuccessful in patients with osteonecrosis of the talus. Moreover, arthroscopic procedures may require longer surgical times, and the procedures themselves demand a significant learning curve on the part of the operating surgeon.
Answers to Your Questions
The following set of questions and answers is intended to provide instruction to the orthopaedic surgeon considering performing ankle fusion arthroscopically but looking for further guidance as to the indications for the arthroscopic approach and best intraoperative practices for ensuring a well-executed procedure.
Who is the ideal candidate for an arthroscopic procedure versus an open approach?
Dr. Carreira: At our institution, the ideal candidate for an arthroscopic procedure is a younger patient (<50 years old) in whom we can expect good compliance with postoperative weight bearing. The arthroscopic approach preserves malleolar anatomy and leads to minimal scarring of the soft tissue envelope, which makes the patient a better candidate for conversion to ankle replacement in the future, if that proves necessary. The technical execution of arthroscopic arthrodesis is facilitated by a patient with minimal deformity, preserved ankle motion, and small or absent osteophytes anteriorly.
What are the indications for proceeding with an open procedure versus using the arthroscopic technique?
Dr. Carreira: Open procedures allow for more predictable deformity correction. With the arthroscopic technique, 10 degrees of varus or valgus deformity is correctible but the degree of correction is highly dependent on the surgeon’s skill and experience. The open technique may also be better if the patient has anterior tibial bone loss or anterior talar extrusion that requires significant posterior bone resection. The open approach may also be an option if more substantial hardware, such as an ankle fusion plate, is being used to provide greater biomechanical stability. If poor compliance with postoperative therapy is anticipated, an open approach with plate and screws may be preferable to the arthroscopic technique, which often involves use of lag screws alone for fixation.
What keys to success can be offered for surgeons new to the arthroscopic technique?
Dr. Carreira: Proper set-up is critical to a successful procedure. We use mechanical distraction, which aids in joint surface preparation. Using a dedicated outflow cannula will help the surgeon with the removal of osteophytes, by providing adequate outflow and preventing cartilage and subchondral bone from clouding the arthroscopic field. A tourniquet should be used to prevent bleeding, which can also make visualization difficult. Proceeding by way of a systematic approach in which synovectomy and excision of anterior osteophytes precedes removal of articular cartilage and subchondral bone enables the procedure to progress in a controlled fashion. It also allows for maintenance of an anatomic perspective, which, in turn, helps in correcting deformity.
Is any special equipment required for joint preparation and/or fixation?
Dr. Carreira: We prefer using larger arthroscopic cameras, burrs, and shavers (> 4.0 mm) because they allow for higher flow rates and more efficient removal of the osteophytes and joint surfaces. A hooded burr may be useful if the burr catches on the opposite surface when preparing the joint. Powered chisels, osteotomes, and gouges may be useful adjuncts in hard bone, and hand tools will enable perforation and fracture of the subchondral bone plate into the deeper cancellous bone. Fluoroscopy is necessary to verify position of the fusion and to facilitate placement of the cannulated screws. A system for distraction of the ankle is necessary to allow for adequate visualization of the joint.
Dominic Carreira, M.D. is a foot and ankle specialist at Peachtree Orthopedics, Atlanta, Ga. He is also founder and president of the Multicenter Arthroscopy Study of the Ankle and Foot (MASTAF) Study Group. Brendan Emmons, B.S. is a student and research coordinator at Peachtree Orthopedics, Atlanta, Ga.