Osteochondral defects of the ankle have been described with several names, including osteochondral lesions, osteochondral fractures, dome fractures, and osteochondritis dessicans. Osteochondral defects typically occur at the bottom bone of the ankle joint, named the talus. They typically result from previous ankle trauma, such as a sprain or ankle fracture.
Office Appointments and Telemedicine with Dr. Carreira

You can also book an office appointment or a telemedicine visit by calling Dr. Carreira’s office at 404-355-0743. Book now.
The talus has limited capacity to repair itself, and patients with chronic pain should be evaluated for these focal areas of cartilage and/or bone loss. X-rays may show injuries at the talar dome, but are limited insofar as bone damage also must be present to detect these injuries radiographically. Magnetic resonance imaging provides more detailed information regarding cartilage injury and other pathologies around the ankle joint.
CT-Scans of Osteochondral Defect of the Talus
Nonsurgical Treatment for Osteochondral Defects
Generally, nonsurgical treatment involves an initial period of no weight bearing with cast immobilization, followed by progressive weight bearing and mobilization to full ambulation by 12 to 16 weeks. A meta-analysis of 14 studies with a total of 201 patients followed for approximately two years showed only a 45% success rate of nonsurgical treatment of grade I, grade II, and medial grade III talar osteochondral lesions.
Surgical Treatment for Osteochondral Defects

Osteochondral grafts used for replacement of both and cartilage defects in the ankle.
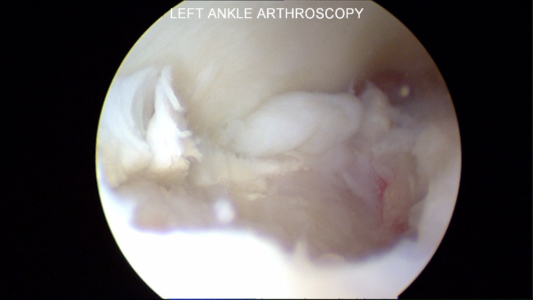
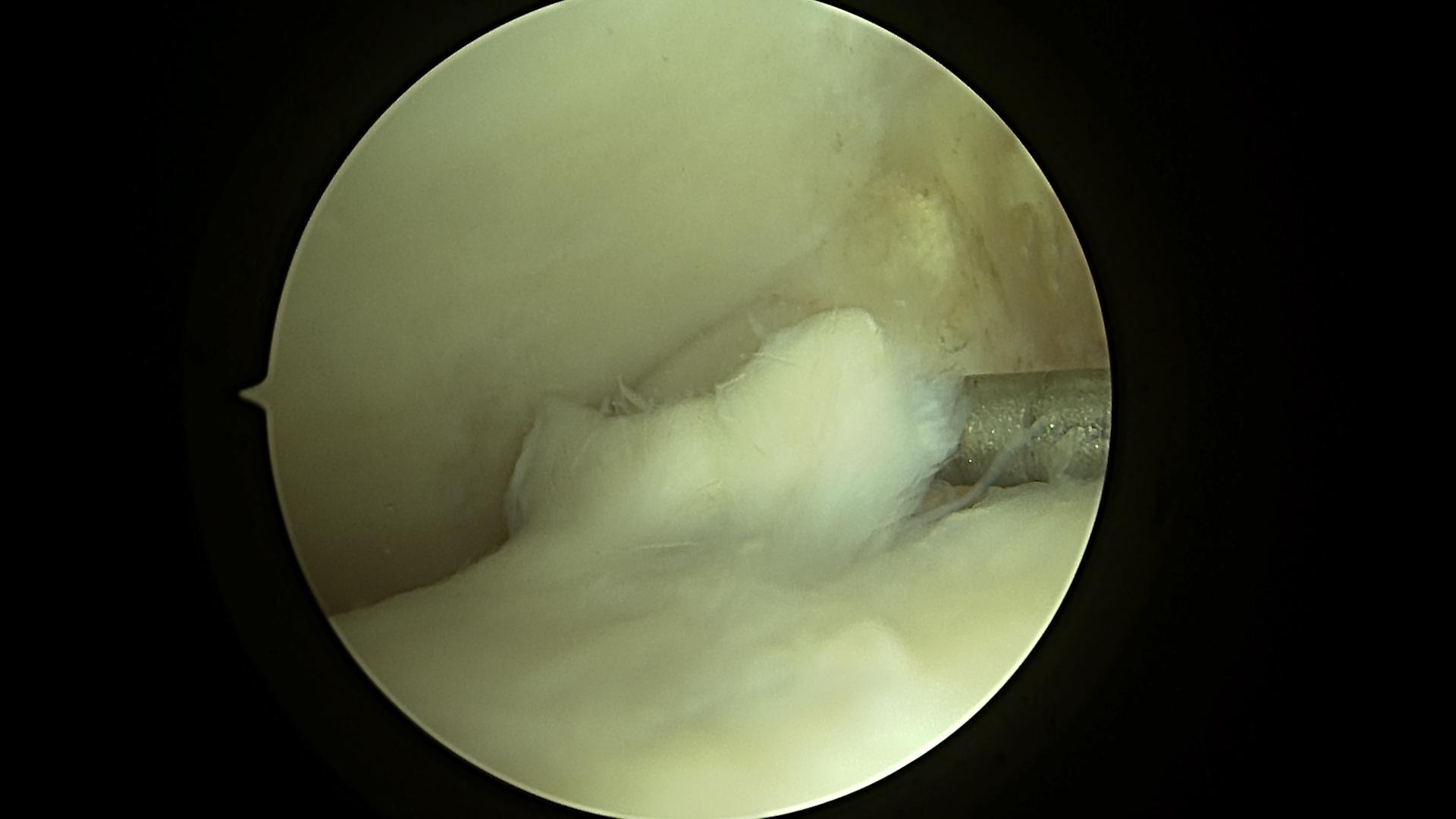
Surgical management is reserved for unstable fragments or for failure of nonsurgical treatment. The first option of surgical treatment is performed with ankle arthroscopy and consists of the microfracture technique or drilling, in which multiple holes spaced 2-3 mm apart are placed into the cartilage defect to stimulate cartilage healing.
Results of microfracture or drilling have been encouraging compared with those of nonsurgical treatment. In a review of 16 studies with a total of 165 patients, Tol et al found these bone marrow stimulating techniques to have had “good-to-excellent” results in 88% of patients with grade III and higher lesions.
As a second and more invasive line of treatment, osteochondral grafting may be performed to reconstruct the talar dome, also leading to high success rates with pain relief and functional improvement.
A third option for acute injuries is internal fixation of osteochondral lesions. This may be done using a variety of methods, including screws, Kirschner wires, and bioabsorbable devices. If sufficient healthy bone forms part of the osteochondral defect, fixating the osteochondral lesion may lead to significant healing.
A Three-Step Surgical Procedure: Microfracture to Treat Ankle Cartilage Defect
Microfracture to Treat Ankle Cartilage Defect – Part 1
Microfracture to Treat Ankle Cartilage Defect – Part 2
Microfracture to Treat Ankle Cartilage Defect – Part 3
You can watch all three videos in this Microfracture to Treat Ankle Cartilage Defect as a playlist on Dr. Carreira’s YouTube channel.
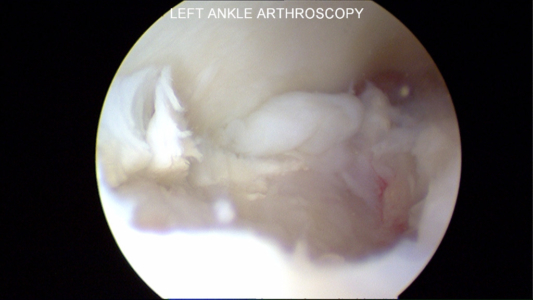
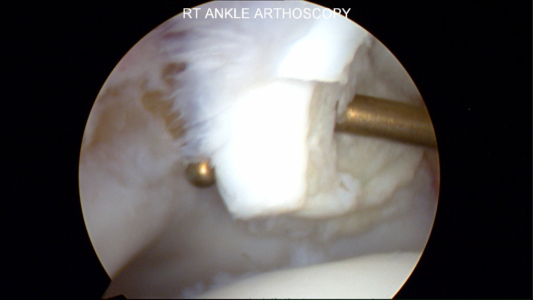
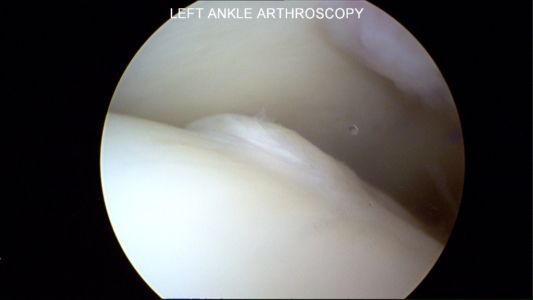
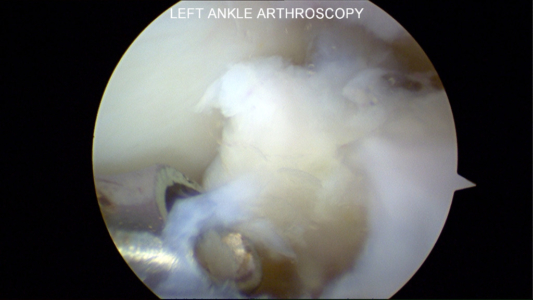
Photos of Surgical Treatment for Osteochondral Defect (Ankle Cartilage Injury)
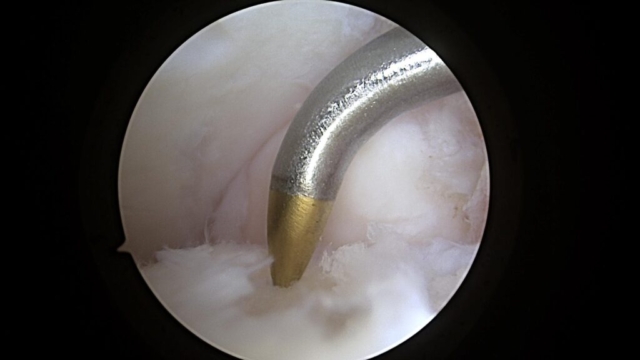
Below are pictures at the time of ankle arthroscopy for the treatment of ankle cartilage injury, also known as an OCD or chondral defect or injury.
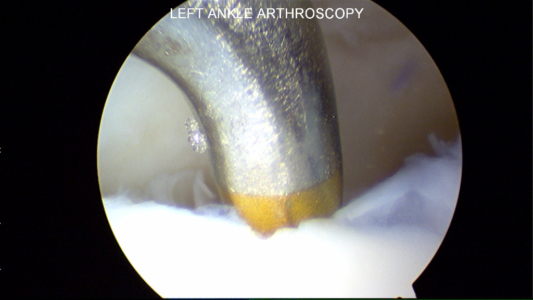
Unstable Cartilage Flap to be Surgically Removed
In this surgical procedure, a metal rod is used to lift the flap of cartilage on the talus and show the unstable cartilage. The cartilage on the top is from the tibia and on the bottom is the talus.
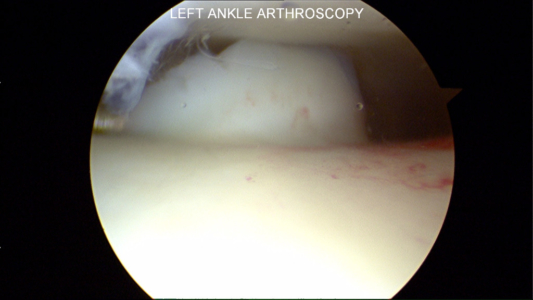
Microfracture Awl to Stimulate Cartilage Healing
Postsurgical Recovery for Osteochondral Defect
Following ankle surgery for osteochondral defects, patients typically are instructed to remain nonweight-bearing for 6 weeks. Ankle range-of-motion is begun at the time of suture removal, typically at two weeks. Patients are placed into CAM boots and are instructed to perform a range of motion exercises at least 3 times per day.
International Consensus Meeting on Cartilage Repair of the Ankle
In November 2017, Dr. Dominic S. Carreira attended the International Consensus Meeting on Cartilage Repair of the Ankle. Organized by the Department of Orthopaedic Surgery at the University of Pittsburgh, this invite-only gathering aimed to foster consensus on key areas within the field of ankle repair.
What follows below is a recap of the questions, answers, and votes that Dr. Carreira and his colleagues on the History, Physical Examination, Imaging and Arthroscopy Section considered, assembled and submitted.
Diagnosis – History, Physical Examination, Imaging and Arthroscopy
1. Which aspect(s) of the patient history can be documented in the setting of a known or suspected cartilage lesion of the ankle?
Answer: The following aspects of the patient history can be documented in the setting of a known or suspected cartilage lesion of the ankle:
- History of trauma
- Mechanism of injury
- Localization of pain
- Mechanical symptoms (e.g., locking, instability)
- Swelling
- Duration of symptoms
- Previous treatment ADLs/sporting activities
Vote: Unanimous
2. Which aspect(s) of the physical examination can be performed/documented in the setting of a known or suspected cartilage lesion of the ankle?
Answer: The following aspects of the physical examination can be performed/documented in the setting of a known or suspected cartilage lesion of the ankle:
- Ankle range of motion
- Tenderness to palpation
- Assessment of stability (e.g., anterior drawer, talar tilt)
- Swelling
- Alignment
Vote: Strong Consensus
3. How can the surgeon clinically discern whether a cartilage lesion of the ankle is symptomatic?
Answer: A clinical history of pain +/- swelling, usually exacerbated with activity, is the most important aspect in discerning whether a cartilage lesion of the ankle is symptomatic.
Vote: Strong Consensus
4. Which radiographic/imaging studies can be utilized to evaluate a known or suspected cartilage lesion of the ankle?
Answer: Weight-bearing AP, lateral, and mortise radiographs can be utilized to evaluate a known or suspected cartilage lesion of the ankle. Standard CT and/or MRI sequences are sufficient to evaluate a known or suspected cartilage lesion of the ankle.
Vote: Strong Agreement
5. Which specific radiographic/imaging protocols can be utilized to evaluate a known or suspected cartilage lesion of the ankle?
Answer: Weight-bearing AP and lateral radiographs can be utilized to evaluate a known or suspected cartilage lesion of the ankle. Standard CT and MRI sequences are sufficient to evaluate a known or suspected cartilage lesion of the ankle. A CT scan with the ankle in full plantar flexion can be ordered to evaluate arthroscopic accessibility for preoperative planning.
Vote: Strong Consensus
6. Which radiographic/imaging findings can be assessed/documented in the setting of a cartilage lesion of the ankle?
Answer: The following radiographic/imaging findings can be assessed/documented in the setting of a cartilage lesion of the ankle:
- Size
- Location
- Stability of the lesion
- Loose fragments
- Cystic changes
- Degenerative changes
- Edema
- Alignment
- Associated lesions/injuries
Vote: Strong Consensus
7. How can the location of a lesion(s) be documented?
Answer: The location of a lesion can be documented using a nine-zone anatomic grid scheme (medial/central/lateral and anterior/central/posterior), as described by Elias et al.
Vote: Strong Consensus
8. How can lesion size be measured on imaging?
Answer: Lesion size can be estimated in three planes, including surface area and depth of the lesion. If precise measurement is required including depth, the use of CT is recommended. For daily practice, a size estimate using MRI is appropriate.
Vote: Unanimous
9. How can lesion size be measured/confirmed during surgery?
Answer: Intra-operative measurement of lesion size can be estimated via the use of a probe in order to confirm the size assessment made via imaging. However, intra-operative measurement of lesion size can be difficult and inaccurate.
Vote: Strong Consensus
10. When is diagnostic arthroscopy a helpful tool in assessing a known or suspected cartilage lesion of the ankle?
Answer: Diagnostic arthroscopy is of limited value and seldom influences treatment approach in the assessment of a known or suspected cartilage lesion of the ankle.
Vote: Strong Consensus
11. What considerations can be made when extrapolating imaging findings to expected surgical findings of a cartilage lesion of the ankle?
Answer: Magnetic resonance imaging tends to overestimate lesion size.
Vote: Strong Consensus
12. How can associated conditions (e.g., ankle instability, peroneal tendon pathology, malalignment, kissing lesions, etc.) be assessed in the setting of a cartilage lesion of the ankle?
Answer: Associated conditions can be assessed clinically with a careful history and physical examination. If indicated, additional imaging studies may include specific radiographic views, ultrasound and/or MRI. It is recommended that specific attention be given to alignment.
Vote: Strong Consensus
Conservative Management and Biological Treatment Strategies of Osteochondral Defect
1. In what cases can conservative management be considered for a cartilage lesion of the ankle?
Answer: Conservative management for cartilage lesions of the ankle can be considered in the following scenarios:
- Asymptomatic lesions
- Incidental findings
- Non-displaced acute bone/cartilage injury
- Older age with lower functional status
- Signs of adjacent joint arthritis
- Skeletally immature patient
Vote: Strong Consensus
2. What prognostic factors can be considered when utilizing conservative management for cartilage pathology of the ankle?
Answer: The following prognostic indicators can be considered when utilizing conservative management for cartilage pathology of the ankle:
- Patient age
- BMI
- Acuity of the lesion
- Size of the lesion
- Location of the lesion
- Presence of cystic change
- Ankle instability
- Evidence of loose body
- Functional status
- Adjacent bone or cartilage lesions
- Medical comorbidities
- Progression of lesion size on imaging
Vote: Strong Consensus
3. What is the optimal protocol for conservative management (e.g., brace, cast, boot, PT, etc.) of a cartilage lesion of the ankle?
Answer: The optimal protocol for conservative management of an acute nondisplaced osteochondral lesion of the ankle is immobilization for 4-6 weeks with touchdown weight bearing. Non-steroidal anti-inflammatory drugs (NSAIDs) can be prescribed in cases of significant pain and swelling unless otherwise medically contraindicated. In cases with a significant bony component to an osteochondral injury, there is no use for a bone stimulator.
Vote: Strong Consensus
4. How can patients be counseled with regards to goals for function after conservative management and how long should they be followed clinically?
Answer: The goal of conservative management should be full return to function with the possibility of some pain with sporting activities. However, patients should be advised to participate in low- impact activities. The duration of treatment for conservative management is highly individualized, but in general, may result in clinical improvement over the course of 3-6 months. If the patient does not demonstrate clinical improvement after 3 months, an MRI should be ordered to re-evaluate the lesion. Overall, the lesion(s) is unlikely to heal and may increase in size; patients should understand the signs and symptoms of progression (swelling, increased pain, mechanical symptoms). Patients should be followed clinically every 6 months.
Vote: Consensus
5. Can the injection of a biological product (e.g., cBMA, HA, PRP, adipose, etc.) be considered as a conservative management strategy for a cartilage lesion of the ankle? If so, when?
Answer: The injection of a biological product in the form of concentrated bone marrow aspirate or platelet-rich plasma can be considered as a conservative management strategy for a cartilage lesion of the ankle if there is no improvement in symptoms after 4-6 weeks.
Vote: Consensus
6. For how long can conservative management be attempted before surgery is recommended?
Answer: The length of conservative management can be based upon symptom progression/regression, as well as size and displacement of the lesion. In general, conservative treatment can be attempted for 3 months before surgery is recommended, with the following exceptions:
- An acute, displaced osteochondral fragment can be fixed immediately.
- Large lesions with edema and/or ligamentous instability should be treated at 6-8 weeks if there is no response to conservative treatment.
In general, conservative management may not be prolonged to 6 months, with the following exceptions:
- A demonstrable improvement in symptoms
- Unresolved/uncontrolled medical co-morbidities
Vote: Strong Consensus
7. Can the injection of a biological product be considered as an adjunct to surgery in cartilage repair of the ankle? If so, when?
Answer: Biologic augmentation in the form of concentrated bone marrow aspirate or platelet-rich plasma can be routinely used as an adjunct to surgery in cartilage repair of the ankle.
Vote: No Consensus
8. What are the potential benefits and limitations to the available biological products for cartilage pathology of the ankle?
Answer: Human cell/tissue products and orthobiologics may improve the quality of the repair of cartilage and improve patient outcomes.
Vote: Strong Consensus
9. Is there an optimal formulation, cell source or cell concentration of the available biological products in the setting of cartilage repair?
Answer: Currently, there is no optimal formulation, cell source, or cell concentration of the available biological products in the setting of cartilage repair.
Vote: Strong Consensus
10. What patient- and product-specific parameters/data points can be recorded when administering a biological product?
Answer: The following patient-specific parameters/data points can be recorded when administering a biological product:
- Patient age
- Anti-platelet agent usage
- Cost
- Medical co-morbidities (e.g. hematological disease)
- Prior treatments
- Characteristics of the lesion
- Smoking status
The following product-specific parameters/data points can be recorded when administering a biological product:
- Product/manufacture
- Centrifuge specifications
The following parameters can be utilized in the standardized assessment of a biological product:
- Cell count
- Cell concentration
- Growth factor count
- Source (e.g., peripheral blood, iliac crest bone marrow, etc.)
Vote: Strong Consensus
11. What risks/benefits can be discussed with patients prior to administering a biological product?
Answer: The following risks/benefits can be discussed with patients prior to administering a biological product:
- Potential for symptomatic improvement
- Potential for pain/tenderness at donor site
- Potential for treatment failure
- Potential for direct patient costs
- Duration of potential relief
- Potential for hyper inflammatory response
- Potential for progression of underlying disease despite pain free state
- Discussion of contemporary research
Vote: Strong Consensus
12. Is there a role for biophysical stimulation (e.g., electric, low-intensity pulsed ultrasound, etc.) as an adjunct to the conservative or surgical treatment of a cartilage lesion of the ankle?
Answer: Presently, there is no role for biophysical stimulation (i.e. electrical stimulation, low intensity pulses ultrasound, etc.) as an adjunct to the conservative or surgical treatment of a cartilage lesion of the ankle.
Vote: Strong Consensus
13. What considerations can be made when choosing between cellular and acellular cartilage products?
Answer: There is not enough data to differentiate between cellular and acellular cartilage products; however, the following parameters can be considered:
- Cost
- Patient age
- Product shelf life
- Prior surgeries
- Size of lesion
- Presence or absence of a cyst(s)
Vote: Strong Consensus
Debridement, Curettage, and Bone Marrow Stimulation
1. In what cases/lesion types can debridement and curettage without bone marrow stimulation be considered for the surgical treatment of cartilage pathology of the ankle?
Answer: Debridement and curettage without bone marrow stimulation can be considered for the following cases/lesion types:
- Partial thickness chondral lesions
- Acute lesions (e.g., found during arthroscopy after ankle fracture; professional athlete in season and looking to return to competition; etc.)
- Incidental lesion found during arthroscopy
- Lesion caused by other disease (e.g., gouty arthritis, PVNS, etc.)
Vote: Strong Consensus
2. In what cases/lesion types can bone marrow stimulation be considered for the surgical treatment of cartilage pathology of the ankle?
Answer: Bone marrow stimulation can be considered for the surgical treatment of full thickness chondral or osteochondral lesions that have failed conservative treatment.
Vote: Strong Consensus
3. What are the ideal lesion size guidelines (diameter, depth, etc.) for the use of bone marrow stimulation in the primary surgical treatment of an osteochondral lesion of the talus?
Answer: The ideal size guidelines for use of bone marrow stimulation are lesions <10 mm in diameter, <100 mm2 in area, and <5 mm in depth. Bone marrow stimulation is less likely to succeed when used as a sole treatment in a lesion 15 mm in diameter or greater.
Vote: Strong Consensus
4. What local prognostic factors should be considered when utilizing bone marrow stimulation for the surgical treatment of cartilage pathology of the ankle?
Answer: The following prognostic factors should be considered when utilizing bone marrow stimulation for surgical treatment of cartilage pathology of the ankle:
- Lesion size
- Lesion location
- Presence of a cyst(s)
- Uncontained lesion
- Bone marrow edema
- Joint alignment
- Ankle stability
- Previous cartilage repair procedure
Vote: Strong Consensus
5. How can the lesion site (base and edge) be prepared prior to bone marrow stimulation?
Answer: The lesion site can be prepared prior to bone marrow stimulation by debriding all loose or fibrillated cartilage until there is a stable rim of articular cartilage. Stable edges should be vertical and 90 degrees to the subchondral bone. The calcified cartilage layer of bone should be removed, but care should be taken not to destroy the framework of the underlying subchondral bone.
Vote: Strong Consensus
6. How can damaged cartilage be differentiated from healthy cartilage intra-operatively and how much should be removed?
Answer: All unstable cartilage can be removed from the defect site. Articular cartilage that is stable, but appears abnormal/damaged, can be left in situ, as stability is more important than visual appearance and slightly damaged but stable cartilage is superior to fibrocartilage. The following methods may be used to differentiate damage cartilage from healthy cartilage intra-operatively:
- Probing articular cartilage to assess how soft or ballotable it is
- Probing articular cartilage to see if it can be delaminated off of subchondral bone
Vote: Strong Consensus
7. Can an awl or drill be utilized for bone marrow stimulation of the ankle, and what size should be used?
Answer: The use of an awl or a low speed drill of 2 mm or less in size is recommended.
Vote: Strong Consensus
8. To what depth can the awl/drill holes be made in the ankle?
Answer: The awl/drill holes can be made to a depth that results in subchondral bone bleeding or presence of fat droplets.
Vote: Strong Consensus
9. What distance should be maintained between the awl/drill holes in the ankle?
Answer: The distance between the awl apertures should be 3 – 5 mm.
Vote: Strong Consensus
10. To what depth can a lesion be debrided before bone grafting is required in the ankle?
Answer: A lesion can be debrided to a depth of 5 mm before bone grafting is required.
Vote: Strong Consensus
12. Can biological augmentation of a bone marrow stimulation procedure be considered?
Answer: Some form of biological augmentation may be beneficial in lesions treated with bone marrow stimulation in the ankle.
Vote: Unanimous
13. Is it necessary to perform bone marrow stimulation for saucer-type lesions of the ankle?
Answer: Bone marrow stimulation can be performed for saucer-type lesions of the ankle. When a clear bone fragment is visible, the fragment can be preserved in cases where the lesion is acute and large enough to accommodate fixation.
Vote: Strong Consensus
14. Can a repeat debridement, curettage and/or bone marrow stimulation procedure be considered? If so, in what cases?
Answer: A repeat debridement, curettage, and/or bone marrow stimulation procedure can be considered in cases where there is reason to suggest incomplete debridement and/or improper technique in the primary case, as well as in cases where the patient is unwilling to undergo a more invasive procedure.
Vote: Strong Consensus
15. Does a previous debridement, curettage and/or bone marrow stimulation procedure affect the outcome of a subsequent procedure?
Answer: A previous debridement, curettage, and/or bone marrow stimulation procedure will affect the outcome of a subsequent bone marrow stimulation and autologous osteochondral transplantation procedure, but not in subsequent cases of allograft or scaffold-based therapies.
Vote: Consensus
Fixation Techniques
1. In what cases/lesion types can fixation be considered for the surgical treatment of a cartilage lesion of the ankle?
Answer: Both acute and chronic lesions are indicated for fixation, and can be considered in the following cases:
- An intact osteochondral fragment larger than 10 mm in diameter
- A bony fragment of at least 3 mm in thickness
- Fixation is contraindicated in the following cases:
- Generalized osteoarthritis
Vote: Strong Consensus
2. Does skeletal maturity play a role in determining whether fixation can be utilized?
Answer: Fixation of a lesion is indicated in a skeletally immature patient when it can be performed without violation of the growth plate and no medial malleolar osteotomy is required.
Vote: Strong Consensus
3. Is there an optimal timeframe after an osteochondral fracture of the talus in which fixation should be performed?
Answer: A symptomatic displaced fragment in all patients or a non-displaced fragment in a skeletally mature patient can be fixed as soon as possible in order to maximize healing potential and minimize intra-articular damage. A symptomatic non-displaced fragment in a skeletally immature patient may undergo conservative treatment for 3-6 months prior to recommending surgery.
Vote: Strong Consensus
4. If the cartilage lesion has expanded and does not fit in the original defect site, can the defect site and/or fragment be shaped to facilitate a fit? If so, how?
Answer: The osteochondral unit can be shaped until it fits the defect site. First, the sclerotic bone should be removed from the defect site, followed by removal of the unstable cartilage from the defect borders. If the cartilage fragment is still too big, it is often the cartilage that has expanded and this can be trimmed away using a blade until the fragment fits.
Vote: Strong Consensus
5. How should the lesion site be prepared prior to fixation?
Answer: Adequate debridement and bone marrow stimulation should be performed prior to fixation. First, all sclerotic bone from the base of the defect should be removed, which can be performed with a curette or shaver. For bone marrow stimulation, the base of the defect can be drilled with a K-wire or small drill bit.
Vote: Strong Consensus
6. Is there a minimum amount of bone required on the fragment side to facilitate fixation?
Answer: The minimum amount of bone required on the fragment side to facilitate fixation is 3 mm in thickness and 10 mm in diameter. However also the shape of the fragment plays an important role here, there is also the option of using 2.0 mm diameter fixation screws.
Vote: Strong Consensus
7. Can fixation be performed in the case of a purely cartilaginous lesion?
Answer: Fixation of a purely cartilaginous lesion is possible, but unlikely to be successful and therefore not recommended.
Vote: Strong Consensus
8. Are there cases in which fixation with bone grafting is required?
Answer: Chronic lesions may require bone grafting in cases where debridement of sclerotic and poorly vascularized bone tissue yields a bone void not conducive to accepting the osteochondral fragment. Lesions that have minimal defect, no cyst and bleeding bone does not require bone grafting.
Vote: Strong Consensus
9. Is there an optimal method of fixation?
Answer: At least one bioabsorbable compression screw is recommended; additional bioabsorbable dart(s) or pin(s) can be utilized to prevent rotation. The alternative is provided with 2.0 or 2.7 mm steel screws for fixation or bone peg.
Vote: Strong Consensus
10. How can the size of fixation device be determined?
Answer: The size of fixation device should not compromise the structural integrity of the fragment. A maximum of 3.0 mm screw can be utilized as the primary bioabsorbable implant; alternatives are 2.0 or 2.7 mm steel screws
Vote: Strong Consensus
11. How many fixation devices should be used per lesion?
Answer: When possible, at least 2 fixation devices should be utilized and oriented in a non-parallel fashion.
Vote: Strong Consensus
12. Should the defect be sealed after fixation? If so, how?
Answer: Sealing of the defect is not necessary after fixation.
Vote: Strong Consensus
13. Do fixation techniques facilitate healing of the cartilage and/or subchondral bone?
Answer: Fixation techniques are likely to facilitate healing of the cartilage and/or subchondral bone.
Vote: Strong Consensus
14. Is it possible to perform fixation after a prior bone marrow stimulation procedure?
Answer: There is no indication to perform fixation after a prior bone marrow stimulation procedure.
Vote: Strong Consensus
15. What options are available in the case of treatment failure after fixation?
Answer: A bone marrow stimulation procedure can be performed in the case of treatment failure in lesions smaller than 15 mm in diameter. In larger defects, available options include osteochondral autograft, bone grafting, ACI, etc.
Vote: Strong Consensus
Osteochondral Autograft
1. In what cases/lesion types can osteochondral autograft techniques be considered for the surgical treatment of cartilage pathology of the ankle?
Answer: Osteochondral autograft techniques can be considered in primary cystic lesions > 1 cm in diameter, as well as in revision scenarios after a failed primary procedure with a lesion size > 1 cm in diameter.
Vote: Strong Consensus
2. What are the prognostic factors that should be considered when performing an osteochondral autograft procedure?
Answer: The most important prognostic factor that should be considered when performing an osteochondral autograft procedure is BMI. The following factors may also be prognostic and may be considered when performing an osteochondral autograft procedure: Concomitant tibial/kissing lesion Joint alignment Lesion location Lesion size Patient age Presence of degenerative joint disease Previous treatment Surgeon experience Ankle stability Lesion containment
Vote: Strong Consensus
3. Can an osteochondral autograft should be performed on an uncontained lesion?
Answer: When indicated, an osteochondral autograft procedure can performed on an uncontained lesion and can achieve expected outcomes.
Vote: Strong Consensus
4. To what degree was congruency of the graft important necessary?
Answer: Congruency of the implanted graft(s) is essential and care should be taken during surgery to achieve an articular surface as closely as possible to the native talus.
Vote: Unanimous
5. What is the optimal depth to drill the lesion site and optimal length of graft to harvest?
Answer: A depth of 12-15 mm is the optimal depth to drill the lesion site and optimal length of graft to harvest.
Vote: Strong Consensus
6. Does the number of grafts required for osteochondral autograft affect clinical outcome?
Answer: The use of two grafts does not have a worse clinical outcome than using one graft, but three or more grafts may negatively affect clinical outcome due to donor site morbidity.
Vote: Strong Consensus
7. In cases where a lesion measures greater than the size of one graft but less than the size of two grafts, how can this scenario be approached technically?
Answer: Two full grafts or overlapping grafts arranged in a half-moon configuration are appropriate technical approaches.
Vote: Strong Consensus
8. Are post-operative cysts a concern after osteochondral autograft procedures? If so, can they be avoided or treated?
Answer: Post-operative cysts are commonly seen following osteochondral autografts, but the extent to which they may affect clinical outcome is unclear. The following methods may be considered as potential means to reduce cyst formation: Ensuring a press-fit construct Prevention of heat necrosis, by using sharp drill bits and low speed Utilizing a biologic to improve healing at the graft-host interface The presence of an asymptomatic cyst in a postoperative patient may not necessarily require further evaluation.
Vote: Strong Consensus
9. Is there a preferred osteochondral autograft donor site?
Answer: The lateral femoral condyle is the preferred osteochondral graft donor site.
Vote: Strong Consensus
10. Is donor site morbidity a concern after osteochondral autograft harvest? If so, can it be reduced?
Answer: The incidence of donor site morbidity after osteochondral graft harvest is generally less than 15%, but warrants concern after graft harvest and should be discussed with patients, particularly in those with a higher BMI and larger lesion size. The following steps are recommended as potential means by which to reduce the incidence of donor site morbidity:
- Early rehabilitation and range of motion of the knee
- Decrease soft tissue manipulation
- Avoid tight closure of lateral capsule
- Avoid iatrogenic damage to the articular cartilage
Vote: Strong Consensus
11. Should the osteochondral autograft donor site(s) be backfilled?
Answer: It is unnecessary to backfill an osteochondral autograft donor site.
Vote: Strong Consensus
12. What consideration(s) can be made when determining a means by which to access the talar dome?
Answer: Choosing a means by which to access the talar dome is dependent upon the location and size of the lesion, as well as ensuring perpendicular access.
Vote: Unanimous
13. Is morbidity of the osteotomy site a concern in the ankle?
Answer: Potential sequelae associated with performing an osteotomy are uncommon and do not warrant concern clinically. However, it is critical to ensure precise technique and reliable fixation of the osteotomy, which includes pre-drilling for hardware fixation, as well as using two parallel screws and a third transverse screw to prevent migration of the osteotomy fragment.
Vote: Strong Consensus
14. Can biological augmentation (e.g., cBMA, PRP, etc.) of an osteochondral autograft procedure be considered?
Answer: Biological augmentation can be considered in an osteochondral autograft procedure.
Vote: Consensus
Osteochondral Allograft
1. In what cases/lesion types can cylindrical osteochondral allograft plugs be considered in preference to autograft for the surgical treatment of cartilage pathology of the ankle?
Answer: Cylindrical osteochondral allograft plugs can be considered in preference to autograft in the following scenarios:
- Contained lesions greater than 1.5 cm in diameter
- Knee osteoarthritis
- History of knee infection
- Patients expressing concern with donor site morbidity of the knee
Vote: Strong Consensus
2. Is it appropriate to utilize osteochondral allograft plugs from the knee or should it be limited to allografts plugs from the talus?
Answer: The allograft should be sourced from the talus, as well as be matched for size and side for reasons relating to cartilage thickness, morphology, and congruency.
Vote: Strong Consensus
3. Is there a use for decellularized osteochondral allograft plugs in cartilage repair of the ankle? If so, in what cases?
Answer: There is an absence of clinical evidence and/or clinical experience to recommend in favor of or against the use of decellularized osteochondral allograft plugs.
Vote: Strong Consensus
4. In what cases/lesion types can bulk osteochondral allograft transplant be considered for the surgical treatment of an osteochondral lesion of the talus?
Answer: Bulk osteochondral allograft transplant can be considered in uncontained/shoulder lesions or lesions that cannot be addressed with an osteochondral autograft.
Vote: Strong Consensus
5. What is the preferred type of allograft (storage, preservation, etc.) for use in the ankle?
Answer: Fresh, non-frozen allograft is preferred for use in the ankle.
Vote: Strong Consensus
6. Is there an optimal time for use of fresh osteochondral allograft? When is it too late to use secondary to loss of chondrocyte viability?
Answer: Fresh osteochondral allografts should not be used if older than 28 days. It is preferable to use grafts not older than 21 days.
Vote: Strong Consensus
7. Can HLA cross-matching and T cell antigenic response be assessed for fresh allografts, and/or should patients and grafts be tested to assess any association with future failure?
Answer: There is an absence of clinical evidence and clinical experience to recommend in favor of or against HLA cross-matching and assessing T cell antigenic responses for fresh talar allografts.
Vote: Strong Consensus
8. Which measurements of the talus are most critical when procuring a sized-matched talus for bulk transplantation?
Answer: Three-dimensional measurements (length, width, and height) of the talus as measured on CT scan are the most critical measurements when procuring a sized-matched allograft for bulk transplantation.
Vote: Unanimous
9. What is the best means of accessing the talar dome for bulk osteochondral allograft transplantation?
Answer: An anterior approach will allow access to the talar dome for bulk osteochondral allograft transplantation in the majority of cases. A transmalleolar or posterior approach can be utilized when necessary.
Vote: Strong Consensus
10. What is the minimum amount of bone stock that should be maintained in the native talus after preparation for a bulk osteochondral allograft transplantation?
Answer: Complete excision of the lesion and a healthy bed of bleeding bone to facilitate healing and fixation are paramount.
Vote: Strong Consensus
11. What is the minimum graft depth that should remain on the bulk osteochondral allograft transplant for treatment of an osteochondral lesion of the talus?
Answer: A minimum of 10 mm of bone should remain on the bulk osteochondral allograft transplant. Grade of evidence: E
Vote: Strong Consensus
12. What is the optimal method of fixation for a bulk osteochondral allograft in the ankle?
Answer: A conformed fit with headless compression screws is the preferred method of fixation for bulk osteochondral allograft in the ankle.
Vote: Strong Consensus
13. How can patients be counseled with regards to goals for post-operative function after bulk osteochondral allograft procedures?
Answer: Bulk osteochondral allograft has the potential to provide significant improvements in ankle pain and function. Patients should refrain from performing impact activities for 1-year post operatively. Over the long-term, patients should maintain low-moderate impact activity and avoid high impact activity.
Vote: Strong Consensus
14. Is graft collapse a concern after bulk osteochondral allograft transplantation? If so, can it be reduced to limit the amount of bone loss in the event that the patient requires a subsequent procedure?
Answer: Graft collapse is a rare cause of failure following bulk allograft transplantation. At the time of transplantation, care should be taken intra-operatively to remove only the amount of bone that is needed to limit the amount of bone loss.
Vote: Strong Consensus
15. Should biological augmentation of an osteochondral allograft procedure be considered?
Answer: Biological augmentation may be considered in conjunction with osteochondral allograft transplantation.
Vote: Strong Consensus
Scaffold Based Therapies
1. In what cases/lesion types can an autologous chondrocyte implantation procedure be considered for a cartilage lesion of the ankle?
Answer: ACI can be considered in primary or revision procedures for large lesions greater than 1 cm2, with or without cysts, including shoulder lesions.
Vote: Strong Consensus
2. Is there an optimal type/composition of scaffold that can be used in an autologous chondrocyte implantation procedure of the ankle?
Answer: The optimal type of scaffold for ACI is a self-adherent scaffold. No optimal composition of scaffold was determined.
Vote: Strong Consensus
3. What is the ideal location for harvesting chondrocytes for ACI?
Answer: There is no ideal location for harvesting chondrocytes, however consideration should be given to harvesting from the talus.
Vote: Strong Consensus
4. In what cases can the addition of a scaffold to bone marrow stimulation (e.g., matrix- augmented bone marrow stimulation) be considered?
Answer: The addition of a scaffold to a bone marrow stimulation (e.g., matrix-augmented bone marrow stimulation) can be considered in the following cases:
- Primary and revision cases with lesions >1 cm2
- Cases in which a one-step procedure is preferred
- In cases where bone grafting may be needed
Vote: Strong Consensus
5. Is there a preferred type/composition of scaffold that can be used with matrix-augmented bone marrow stimulation?
Answer: There is no preferred type/composition of scaffold for use with matrix-augmented bone marrow stimulation.
Vote: Unanimous
6. Should scaffolds be fixed to the site of the lesion? If yes, what is the optimal method(s) for fixation?
Answer: Yes, a scaffold should be fixed to the site of the lesion using fibrin glue.
Vote: Strong Consensus
7. Can a scaffold be utilized for an uncontained lesion?
Answer: Yes, a scaffold can be utilized for an uncontained lesion with acceptable results.
Vote: Strong Consensus
8. What amount of bone loss necessitates grafting of a defect prior to utilizing a scaffold?
Answer: Bone grafting may be considered in cases with > 3mm of bone loss, as measured intraoperatively following debridement. The amount of bone graft needed is the amount necessary in addition to the scaffold to fill the defect.
Vote: Strong Consensus
9. Should the addition of an orthobiologic(s) to a scaffold be considered?
Answer: Orthobiologics can be added to all scaffold-based procedures.
Vote: Strong Consensus
Subchondral Pathology
1. In what cases/lesion types can retrograde drilling of the ankle be considered?
Answer: Retrograde drilling (RD) of the ankle can be considered in cases of isolated subchondral lesions, with or without subchondral cyst, and intact overlying articular cartilage when assessed arthroscopically.
Vote: Strong Consensus
2. What technical considerations can be utilized for targeting and drilling a subchondral lesion of the ankle?
Answer: Intra-operative imaging and/or a targeting device may be useful for ensuring accurate placement of the guidewire and preventing penetration of the intact cartilage.
Vote: Strong Consensus
3. What size drill can be utilized for retrograde drilling of a subchondral lesion of the ankle?
Answer: A 1 – 2 mm size K-wire can be utilized for retrograde drilling of a subchondral lesion of the ankle. Care should be taken to not over drill the subchondral lesion and cause iatrogenic damage to the subchondral bone.
Vote: Strong Consensus
4. Should computer-aided navigation/robot-assisted surgery be utilized when performing retrograde drilling for a subchondral lesion of the ankle?
Answer: It is unnecessary to use computer-aided navigation/robot-assisted surgery when performing retrograde drilling for a subchondral lesion of the ankle.
Vote: Strong Consensus
5. Does bone marrow edema of the ankle require treatment?
Answer: Asymptomatic bone marrow edema of the ankle should always be treated conservatively. Symptomatic bone marrow edema of the ankle without an identifiable cartilage or subchondral bone lesion warrants conservative treatment for a minimum of 3 months. A 4-6 week period of non-weightbearing and a course of anti-inflammatory medication should be considered. If symptoms continue beyond 3 months, a repeat MRI should be obtained and in the setting of a persistent or progressive lesion, retrograde drilling can be considered.
Vote: Strong Consensus
6. Can commercially available bone void substitutes be considered as a surgical treatment for subchondral bone marrow lesions of the ankle?
Answer: Cancellous bone grafting is the preferred method of treatment in cases of subchondral bone marrow lesions of the ankle. There is no evidence for or against bone void substitutes.
Vote: Strong Consensus
7. For what types of lesions can bone grafting be considered?
Answer: Bone grafting can be utilized in cases of lesions with large subchondral cysts, as well as in cases with large and/or deep lesions with or without subchondral cysts. Lesions with a diameter > 1 cm, depth > 1 cm and cysts > 100 mm3 require bone grafting. For cystic lesions, bulk bone transplantion (e.g., osteochondral autograft/allograft) should be considered.
Vote: Strong Consensus
8. In what cases can antegrade cancellous bone transplantation be considered?
Answer: Antegrade cancellous bone transplantation can be considered as a treatment option in cases with large, cystic lesions with concomitant articular cartilage damage of the anterior and central aspects of the talar dome that can be approached without osteotomy when placing the ankle in plantarflexion.
Vote: Strong Consensus
9. In what cases can retrograde cancellous bone transplantation be considered?
Answer: Retrograde cancellous bone transplantation can be considered as a treatment option in cases with large, cystic lesions of the posterior aspect of the talar dome or a shoulder lesion that would otherwise require osteotomy.
Vote: Strong Consensus
Revision and Salvage Management
1. How can treatment failure be defined and what are the diagnostic criteria in the setting of cartilage repair of the ankle?
Answer: Treatment failure of cartilage repair of the ankle can be considered in any of the following circumstances 1 year after surgery in the absence of additional ankle injury:
- Persistent pain or symptoms that interfere with desired patient activities correlating to the treated lesion(s)
- Persistent lesion(s) on imaging in symptomatic patients
- No improvement or a decline of patient reported outcome score(s) compared to the pre-operative baseline
- Treatment failure of cartilage repair of the ankle is considered if a revision surgery is performed for the primary lesion.
Vote: Strong Consensus
2. When can a revision procedure be performed in the setting of a failed primary cartilage repair procedure of the ankle?
Answer: Revision surgery can be considered when a failed primary cartilage procedure has been identified as the source of patient symptoms, in the absence of severe degenerative joint disease. Revision surgery can be considered when there is a tangible cause for failure and conservative treatment is unlikely to improve patient outcomes.
Vote: Strong Consensus
3. What factors should be considered in determining the choice of revision procedure in the setting of cartilage repair of the ankle?
Answer: The following factors should be considered in determining the choice of revision procedure in the setting of cartilage repair of the ankle:
- Appearance of the lesion on imaging
- Mechanical factors (e.g., instability, malalignment)
- Patient age
- Presence of additional cartilage pathology
- Presence of a cyst
- Progression of the lesion
- Size of lesion
- Type of initial procedure
Vote: Strong Consensus
4. How does a previous procedure impact the results of a subsequent revision procedure in the setting of cartilage repair of the ankle?
Answer: Any previously performed cartilage repair procedure may negatively impact the results of a subsequent revision procedure.
Vote: Strong Consensus
5. In what cases can it be contraindicated to perform a revision procedure in a patient who meets the definition of treatment failure in the setting of cartilage repair of the ankle?
Answer: It may be contraindicated to perform a revision procedure in a patient who meets the definition of treatment failure in the following scenarios:
- Current or recent joint infection
- Extensive degenerative joint disease
- Uncontrolled inflammatory arthritis
- Severe stiffness
- Substantial discrepancy between clinical symptoms and imaging findings
- Unrealistic patient expectations beyond which can be met with revision surgery
- Patient noncompliance
Vote: Strong Consensus
6. What different/additional considerations can be made in the evaluation of a failed revision procedure in the setting of cartilage repair of the ankle?
Answer: The following considerations can be made when evaluating a failed revision procedure:
- Active smoker
- Adjacent joint disease
- Assessment and medical comorbidities
- Determine a logical reason for failure
- Evaluation of the subchondral bone
- Joint alignment/instability
- Patient age
Vote: Strong Consensus
7. When is it necessary to consider a salvage procedure (e.g., ankle arthrodesis, total ankle arthroplasty) in the setting of cartilage repair of the ankle?
Answer: It is necessary to consider a salvage procedure in a symptomatic patient with one or more of the following:
- Failed cartilage procedure that cannot be realistically addressed with a revision cartilage procedure
- Progressive osteoarthritis of the joint
Vote: Unanimous
8. What criteria can be utilized in the development of an algorithm to assist clinicians in approaching treatment failure and revision/salvage surgery for cartilage repair of the ankle?
Answer:
- Bipolar lesion
- Condition of the subchondral bone
- Degree of osteoarthritis
- Imaging (extent, evolution and edema)
- Joint alignment and instability
- Patient age
- Patient symptoms
- Previous treatment failure(s)
- Size, location and type of lesion
- BMI
Vote: Strong Consensus
Rehabilitation and Return to Sports
1. What are the general concepts and time points to consider in patients returning to activities of daily living, recreational and/or elite athletic activities after cartilage repair of the ankle?
Answer: The general concepts of rehabilitation to consider in returning patients to activities of daily living, recreational and/or elite athletic activities after cartilage repair of the ankle are:
- Allowing biological healing by limiting shear forces
- Progression of activities based on a clinical evaluation
The following aspects of the clinical evaluation can be utilized when deciding whether to progress rehabilitation activities:
- Pain
- Swelling
- Stability
- Proprioception
In general, shear forces should be limited for 3 months, at which time rehabilitation/training can be progressed. Sport specific training is considered 3-6 months after surgery, and is individualized depending on the type of procedure. Return to competition after cartilage repair of the ankle is considered 6 months to 1 year after surgery, and is individualized depending on the type of procedure.
Vote: Strong Consensus
2. What procedure specific advice can patients be given with regards to their likelihood of returning to sport at the previous level of athletic play after ankle cartilage repair?
Answer: There are no validated specific recommendations to consider for rehabilitation and return to sports after cartilage repair of the ankle. Advising patients with regards to their likelihood of returning to sports at the previous level of athletic play is individualized. It can be conveyed that pain and function are likely to improve with diligent rehabilitation. When available, data from a representative population should be provided to the patient in order to quantify likelihood of returning to sport at the previous level. The following prognostic factors should be used to identify athletes MORE likely to return to the previous level of athletic play:
- Younger age
- Primary procedure
- Lesion size less than 1 cm2
- Previous involvement in a high level and frequency of competition with a strong desire to return
- Low fear of re-injury (e.g., psychological readiness to return to sports)
- Patient compliance
- Biomechanics (e.g., stability, alignment)
Vote: Strong Consensus
3. What effect(s) do concomitant procedures (e.g., osteotomy, lateral ligament reconstruction) have on the overall process of rehabilitation and return to sports after cartilage repair of the ankle?
Answer: The rate limiting factor in the process of rehabilitation is limited by the procedure that requires the most protection, which is most often the cartilage repair procedure. Thus, concomitant procedures typically have no impact on return to sport after cartilage repair of the ankle, but procedure specific impairments related to the concomitant procedure may need to be addressed in the rehabilitation program. In cases of osteotomy, weight-bearing may be delayed to allow time for bone healing. It is important for the surgeon and physical therapist to communicate such that both are fully aware of concomitant procedures performed and the potential surgeon specific implications on rehabilitation activities and associated precautions.
Vote: Strong Consensus
4. Is there a benefit(s) to early versus delayed weight bearing after cartilage repair of the ankle?
Answer: Early weight-bearing is beneficial, so long as shear forces are minimized, and should be utilized after cartilage repair of the ankle. Early weight-bearing is defined as beginning at 4 weeks post-operatively.
Vote: Strong Consensus
5. Is there a benefit(s) to early versus delayed motion after cartilage repair of the ankle?
Answer: Early motion is beneficial and should be utilized after cartilage repair of the ankle. Early motion can begin within 1 week following surgery and should consist of free, active range of motion. Maneuvers such as forced passive movements that extend the patient beyond their available range of motion should be avoided.
Vote: Strong Consensus
6. What criteria can be utilized in the clinical decision making process of clearing an athlete to return to play after cartilage repair of the ankle?
Answer: The following clinical criteria can be utilized in the clinical decision making process of clearing an athlete to return to play after cartilage repair of the ankle:
- Lack of negative effects with impact/loading
- Pain
- Physical function testing assessed in comparison to the contralateral (healthy) limb
- Sport specific tasks at 100% in an unopposed setting
- Strength
- Swelling
The following procedure-specific criteria should be utilized in the clinical decision making process of clearing an athlete to return to play after cartilage repair of the ankle:
- Size of lesion
- Type of lesion (e.g., chondral vs. osteochondral)
- Type of procedure
It is not necessary to utilize imaging in the decision-making process of clearing athlete to return to play after cartilage repair of the ankle.
Vote: Strong Consensus
7. For how long after returning to play following cartilage repair of the ankle should an athlete be advised to follow-up with the surgeon clinically?
Answer: An athlete can be advised to follow-up with the surgeon clinically for a total of 2 years after cartilage repair of the ankle. Further follow-up beyond 2 years is ideal, but only necessary in cases where the patient is or becomes symptomatic.
Vote: Strong Consensus
8. Should psychological factors be considered in the process of rehabilitation and return to sport in athletes? If so, how?
Answer: Yes, psychological factors can be considered in the process of rehabilitation and return to sport in athletes and should be assess by a trained sports psychologist and/or via the mental health/psychological components of the Short Form 12 or 36 questionnaires. This should be assessed pre-operatively for baseline, as well as at routine post-operative intervals in conjunction with post-treatment outcome scores.
Vote: Strong Consensus
9. Are there special considerations to be made in the process of rehabilitation and return to sports in elite athletes?
Answer: Close and frequent communication should occur between the surgeon, athlete and support group around the athlete, with the team athletic trainer or physiotherapist acting as the point person for these discussions given that they work most closely with the athlete on a daily basis. It is imperative that the athlete not be overly aggressive in the process of rehabilitation of cartilage repair of the ankle, as biological healing must be allowed to occur. Elite athletes may proceed through the later phases of rehabilitation at an increased rate secondary to their body awareness and skilled movement patterns, but this should not be influenced by outside circumstances such as time of season, in addition to pressure from coaches, management or agents.
Vote: Strong Consensus
Post-Treatment Follow-Up, Imaging and Outcome Scores
1. How can treatment success be defined?
Answer: Treatment success can be defined using the following parameters:
- Absence of pain
- Patient satisfaction
- Return to work at pre-injury level
- Return to sports at pre-injury level
- Improvement in a pre-treatment patient reported outcome measurement
Vote: Strong Consensus
2. Are there specific patients that need longer follow-up?
Answer: Specific patient scenarios that need longer follow-up include:
- Larger lesions (>15 mm) on imaging
- Lesions of the tibial plafond
- Persistent ankle pain
- Degenerative changes on radiographic imaging
Vote: Strong Consensus
3. Which aspect(s) of the physical examination can be performed/documented on patients after treatment of a cartilage lesion of the ankle?
Answer: The following aspects of the physical examination can be performed/documented on patients after treatment of a cartilage lesion of the ankle:
- The ability to bear full weight on the ankle joint with/without pain
- Range of motion
- Presence of an ankle effusion
- Tenderness to palpation of the ankle
Vote: Strong Consensus
4. For database purposes, patient reported outcome data can be collected after treatment of an osteochondral lesion of the ankle at what post-treatment intervals?
Answer: For database purposes, patient reported outcome data can be collected at the 3, 6, 12 and 24- month time points after treatment of a osteochondral lesion of the ankle and annually thereafter.
Vote: Strong Consensus
5. How can patient reported outcome scores be assessed after treatment of an osteochondral lesion of the talus?
Answer: Patient reported outcomes can be assessed using a validated scoring system.
Vote: Strong Consensus
6. What parameters can be included in an ideal outcome score for cartilage repair of the ankle?
Answer: An ideal outcome score for cartilage repair of the ankle can include the following parameters:
- Pain
- Return to ADLs and/or sports
Vote: Strong Consensus
7. How does the treatment of concomitant pathology (e.g., ankle instability) affect clinical outcome and the choice of outcome score(s)?
Answer: Concomitant pathologies, such as ankle instability, do affect clinical outcomes negatively and should be treated simultaneously if symptomatic. In these cases, it is not necessary to extend the follow-up period beyond 24 months, and the AOFAS score can be used for evaluation.
Vote: Strong Consensus
8. Should radiographic/imaging studies be obtained on patients after treatment of an osteochondral lesion of the ankle? If so, which studies and which specific imaging protocol(s)?
Answer: If treatment of an osteochondral lesion of the talus includes bone grafting or osteotomy(ies), post-operative radiographs should be obtained. In symptomatic patients after treatment of an osteochondral lesion of the talus, post-operative cross-sectional imaging can be indicated.
Vote: Strong Consensus
9. Which radiographic/imaging findings can be assessed/documented after treatment of a cartilage lesion of the ankle?
Answer: On standard radiographs, the following radiographic findings can be assessed/documented after treatment of a cartilage lesion of the ankle:
- Bone healing (e.g., osteotomy)
- Joint congruency
- Stability in cases of an implant (e.g, HemiCAP)
On MRI, the following radiographic findings should be assessed/documented after treatment of a cartilage lesion of the ankle:
- Size and location of the lesion
- Presence of a cyst(s)
- Subchondral bone marrow edema
- Integrity of the overlying cartilage
- Integration of the graft(s)
Vote: Strong Consensus
10. What procedure-specific considerations can be made when evaluating post-treatment imaging?
Answer: In cases of bone marrow stimulation, MRI will demonstrate a hypo intense signal of the regenerated fibrocartilage. In case of autologous osteochondral transplantation (OATS), MRI will demonstrate edema of the subchondral bone for an extended period of time.
Vote: Strong Consensus
11. For how long after cartilage repair of the ankle can clinicians and radiologists agree that there will be expected visualization of post-operative subchondral edema on imaging?
Answer: In asymptomatic patients, post-operative subchondral edema may be seen on imaging for up to two years after treatment.
Vote: Strong Consensus
12. Does clinical function correlate with the appearance of post-treatment imaging?
Answer: Clinical function does not correlate with the appearance of post-treatment imaging except in cases where there is a mechanical cause for symptoms (e.g., loose body or chondral flap).
Vote: Strong Consensus