Hallux Rigidus (Big Toe Arthritis)
Hallux rigidus (hallux limitus is the term used by many podiatrists) is degenerative arthritis of big toe. The most common site of arthritis in the foot is at the base of the big toe. This joint is called the metatarsophalangeal, or MTP joint. It is important because it has to bend every time you take a step. If the joint starts to stiffen, walking can become painful and difficult.
Office Appointments and Telemedicine with Dr. Carreira

You can also book an office appointment or a telemedicine visit by calling Dr. Carreira’s office at 404-355-0743. Book now.
In the MTP joint, in addition to the damage of the articular cartilage at the ends of the bones, a bone spur may develop on the top of the bone, which can cause stiffness and pain, particularly with certain types of shoe wear. Prominence of the bone spurs, as seen in the clinical pictures below, can also cause pressure and pain related to shoe wear.
Hallux rigidus usually develops in adults between the ages of 40 and 60 years. The exact cause is oftentimes not easily apparent.
It has a prevalence of 2.5% in patients over the age of 50, and can be treated with both conservative and surgical intervention. Non-operative management includes use of NSAIDs, activity modification, orthoses, a rigid sole shoe, and injections. Hallux rigidus is classified as grade 1, 2 and 3 in severity based on x-ray findings as defined by Coughlin & Shurnas.
Operative Considerations for Hallux Rigidus
Operative considerations for managing this condition are:
- Cheilectomy with or without osteotomies;
- Interpositional arthroplasty; and
- Fusion.
Cheilectomy
In those patients who prefer to preserve the joint and have grade 1-3 hallux rigidus and have failed nonop treatments, cheilectomy is an option for treatment.
Cheilectomy consists primarily of removing bone spurs and cleaning the joint of any loose cartilage and inflammation
There are 2 options related to the approach in which a cheilectomy can be performed.
Open Cheilectomy
The traditional approach is open and for more advanced and larger sized bone spurs, this is still Dr. Carreira’s preferred technique.
Specific Post Operative Course for Open Cheilectomy
Day 1
- Foot wrapped in bandage and placed in postoperative shoe
- Ice, elevate, and take pain medication
- Expect numbness in foot for 12 24 hours
- Partial weight-bearing
Day 3-5
- The postoperative shoe may be removed at night depending on comfort level
- Ice and elevate as much as possible
- Remove dressings in office and place a light dressing
- Begin frequent range-of-motion exercises
- Physical therapy to regain movement
Week 3
- Begin use of rigid soled shoe
- Continue stretching exercises of the big toe, 3x day for 10 minutes at a time
Arthroscopic Cheilectomy
NOTE: This video includes footage of an arthroscopic surgery.
Arthroscopic cheilectomy is a less invasive option which has the advantages of less scarring, less pain, a lower infection rate, and a quicker recovery. Dr. Carreira has published a book chapter on arthroscopic treatment of the hallux for arthritis, has created a video technique presentation for orthopedic surgeons through the AAOS, and has presented at an international conference recently related to the technique.
Incisions for Arthroscopic Cheilectomy

Note the red arrows in the above photo which indicate the incisions for arthroscopic cheilectomy.
Specific Post Operative Course for Arthroscopic Cheilectomy
Day 1
- Foot wrapped in bandage and placed in postoperative shoe
- Ice, elevate, and take pain medication
- Expect numbness in foot for 12 24 hours
- May fully weight-bear
Day 3-5
- The postoperative shoe may be removed at night depending on comfort level
- Ice and elevate as much as possible
- Replace dressings in office
- Begin frequent range-of-motion exercises
Week 1
- Begin transition into a rigid soled shoe such as a sneaker
- Continue stretching exercises of the big toe, 3x day for 10 minutes at a time
- Physical therapy to regain movement and help with home exercise program (HEP)
Video of Bone Spur Removal for Treatment of Big Toe/Hallux Arthritis (Cheilectomy)
Photo of Soft Tissue Impingement and Synovitis
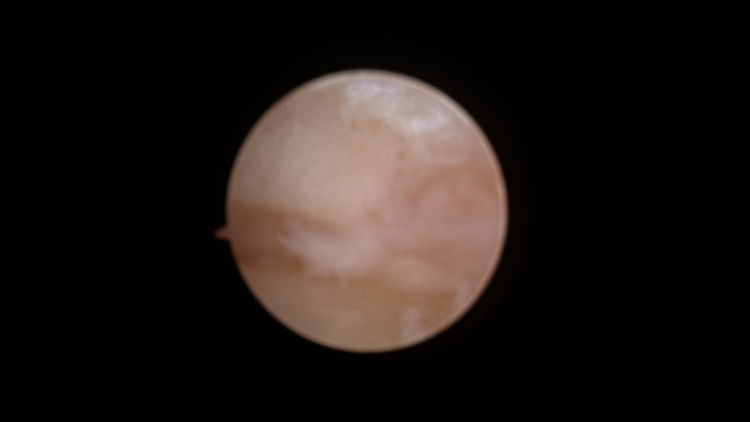
Soft tissue impingement and synovitis observed during arthroscopic cheilectomy of the hallux. The surgical procedure was undertaken to correct big toe arthritis (hallux rigidus).
More of Dr. Carreira’s videos about ankle arthroscopy are available on Dr. Carreira’s YouTube channel.
Medical Research Around Hallux Rigidus
Arthroscopic intervention in cases of hallux rigidus (big toe arthritis) is a developing technique in foot surgery, which has been shown to have good outcomes in peer-reviewed publications. Some evidence for this technique was published in the following studies:
Hickey et al., European Journal of Orthopedic Surgery and Traumatology, 2020
In this study of 36 patients, arthroscopic cheilectomy was performed as the primary procedure to treat of hallux rigidus. At an average follow-up time of 4.7 years, 84% of patients reported no pain or mild pain. None of the patients in this study required big toe fusion down the line.
Iqbal & Chana, Arthroscopy, 1998
This study tracked 15 patients undergoing arthroscopic cheilectomy for treatment of hallux rigidus. At a follow-up point of less than a year (9.4 months), it showed complete pain relief in 67%, partial pain relief in 33% of patients.
Davies & Saxby, JBJS, 1999
This study tracked 12 patients with hallux rigidus and/or osteochondral defects (bone and cartilage injuries) in the great toe. Procedures included arthroscopic cheilectomy, synovectomy (removal of inflamed soft tissue), and osteochondral defect debridement (cleaning up damaged areas). At an average follow-up of 19 months, all patients in this study had no or minimal pain.
Kuyucu et al., Journal of Orthopedic Surgery and Research, 2017
In this study, the authors report results from 14 patients after treatment with cheilectomy, synovectomy, debridement, and microhole drilling. All had significant increases in functional ability, with rapid relief of pain and quick return to activities.
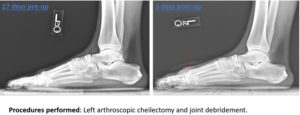
Post-operative x-rays demonstrate elimination of the dorsal spurs on the lateral view.