From his offices in Atlanta, Georgia, Dr. Dominic Carreira has performed approximately 3,200 hip arthroscopies for a variety of diagnoses. The techniques of hip arthroscopy have developed especially over the past 15 years, and these developments have led to significant improvements in patient outcomes.
Length of Hospital Stay: Outpatient or 23 hour admission
Length of Procedure: Approximately 2 hours
Anesthesia: General with a regional lumbar plexus block
What is Hip Arthroscopy?
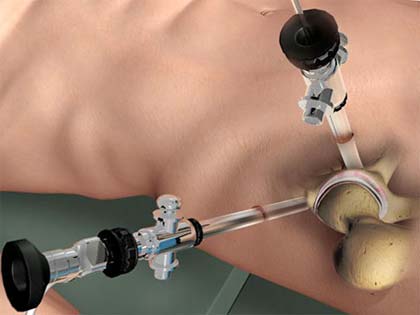
Hip arthroscopy is performed through small approximately one centimeter incisions (typically two or three) using a camera to visualize the inside of the joint. Instruments are inserted through these small incisions to perform the work.
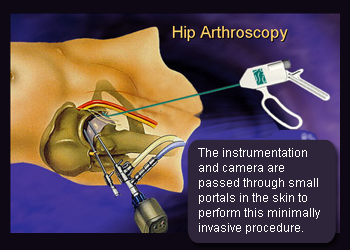 The benefits of hip arthroscopy over open surgery include earlier rehabilitation, an accelerated rehabilitation course, less pain and blood loss, and a lower rate of infection.
The benefits of hip arthroscopy over open surgery include earlier rehabilitation, an accelerated rehabilitation course, less pain and blood loss, and a lower rate of infection.
In the past, diagnosing hip injuries was difficult and the treatment options were limited. Now, advanced diagnostic imaging and a better understanding of pathologies such as labral tears and femoroacetabular impingement have led to more accurate diagnoses, some of which can be treated through an arthroscopic approach.
A number of different pathologies may be treated with hip arthroscopy, including snapping hip, trochanteric bursitis, labral tears, focal chondral injuries, and femoroacetabular impingement. Hip arthroscropy can offer improvements for a number of hip problems.

This photo demonstrates the c sign, which is the letter formed by the thumb and fingers when demonstrating the area of hip pain. This is the most common description for hip pain, and is often described as “deep inside.”
The typical patient who may benefit from hip arthroscopy is suffering from hip pain and does not have a diagnosis of hip arthritis. Arthritis is defined as generalized or diffuse articular cartilage injury of a joint. Hip pain typically occurs in the front and/or the side of the joint, and may also be present in the buttock. Rarely hip joint pain occurs only in the buttock. Patients may experience pain with movement of the hip joint, including flexion, such as when tying shoes or getting into a car, or at rest, such as when sitting or trying to sleep.
The majority of patients, as noted in our MASH study group of over 2500 patients, have a gradual onset of pain without a history of trauma or injury. Patients generally have “normal” X-rays that do not show any signs of arthritis. On close review of these X-rays however, forms of femoroacetabular impingement (FAI) may exist. MRI typically is performed to detect labral tears, which are a common cause of chronic pain in the hip joint.
Patients typically experience increased pain with increased activity, either during the activity itself or in the day or two following the activity.
Hip Arthroscopy Procedure Overview
Arthroscopy: Differences Between Males and Females
There are a number of important differences between males and females undergoing hip arthroscopy. These differences are important for hip arthroscopists to be aware of, as they may affect diagnosis and surgical decision making.
A large multicenter study group of eight arthroscopic hip surgeons collected data on 1437 patients over the course of three years. The findings from that study included the following:
- Females undergoing hip arthroscopy were more likely than males to have greater pain and functional deficits before surgery – as well as increased range of motion.
- On the other hand, males were more likely to have a larger deformity of the head of the femur than were females (i.e. cam impingement.)
- Males and females do not differ in terms of duration of symptoms or location of pain prior to surgery.
Videos of Hip Arthroscopy
To help his patients learn more about potential surgical options, Dr. Carreira has made a number of videos to give his patients some insight into hip arthroscopy.
In the video below, Dr. Carreira offers some insight into the benefits of hip arthroscopy, especially in younger patients.
In this next series of videos, Dr. Carreira describes a number of surgical treatments involving hip arthroscopy.
All Arthroscropic Allograft Labral Reconstruction of the Hip
In March 2014, Dr. Carreira delivered a presentation to the American Academy of Orthopedic Surgeons focused on his unique approach for using a shuttle technique using allograft fascia lata in cases where acetabular labrum tears are irreparable.
These videos are also available on Dr. Carreira’s YouTube channel.
Risks of Hip Arthroscopy
There are several risks to any surgery that must be taken into account. The main risks associated with hip arthroscopy are below:
Infection
The risk of infection is very low and is decreased with a sterile operating environment and antibiotics, as well as careful handling of the incision sites following surgery. Signs and symptoms of an infection are redness, pain, swelling and warmth around the incisions and non-clear drainage from the incision. These infections are typically superficial and require cleaning with soapy water and occasionally antibiotics.
DVT (Deep Vein Thrombosis, blood clot)
The risk of developing a DVT is decreased by starting early motion including the CPM, ankle pumps, aspirin or other blood thinner. Early movement with walker/crutches (not lying in bed immobilized) helps to prevent clots. Signs and symptoms of a blood clot are pain and swelling most commonly in the calf. The calf may also become red and warm to the touch.
Pain
We try to minimize pain as much as possible both in the short and long term, with a goal of little to no pain with full activities after a few months. Medication, ice, rest and therapy reduce post-operative pain. Following restrictions after surgery help to ensure adequate healing of the tissues. ”Little old grandma or grandpa level of activity” in the first 6 weeks is recommended.
Numbness
With hip arthroscopy, there is a very small chance of numbness in the groin and genitalia region and lower extremities post-operatively. You may also experience numbness of the upper outer portion of the thigh on the operative leg after surgery. The lateral femoral cutaneous nerve is close to the surgical area and it may be stretched or bruised during the procedure. Numbness very commonly resolves and Dr Carreira is not aware of any permanent nerve injuries in the patients that he has treated.
Prior to Surgery
Medication
All blood thinning medications (Plavix, Eliquis, Coumadin, Xarelto, Aspirin etc.) need to be stopped prior to your surgery. Appropriate precautions are taken while you have stopped taking these medications. Check with your prescribing physician to see what steps need to be taken when stopping blood thinners.
Discontinue ALL anti-inflammatories at least 7 days prior to your surgery. This includes aspirin, Motrin, ibuprofen, Aleve, naproxen, diclofenac, Celebrex, Mobic.
Discontinue ALL herbal medications at least 7 days prior to your surgery. This includes Turmeric, St. John’s Wort, Gingko Biloba, Ginseng, Garlic, Ephedra, Kava, Valerian, and Echinacea.
Hair removal
You may shave the area around the hip including the pubic hairs to prevent the painful removal of surgical bandages postoperatively. Please shave at least two days before surgery to prevent any open skin cuts at the time of surgery.
Illness
If you begin to feel symptoms of a cold or flu prior to surgery, including a runny nose, cough, or fever, please notify Dr. Carreira’s office. It is possible that your surgery may be postponed.
Equipment
The hip brace, crutches and/or walker will be supplied to you at your pre-op appointment. The CPM will be delivered to your house by 1 – 2 days before the procedure. You will receive the anti- rotation boots on the day of surgery.
After Hip Arthroscopy Surgery
Call our office (404) 355-0743 or proceed to an emergency room if any of the following occur:
- Fever (temperature greater than 101.5°), chills, or sweats
- Increased redness, swelling, or warmth around the incision(s), non-clear (yellow or green) drainage from the incision, or increased pain in or around the incision
- Calf swelling, redness, pain or warmth
- Chest pain, difficulty breathing, or persistent cough
- Excessive bleeding from the incision (you needed to change the dressing twice in a 12 hour period) or foul odor
Post-op Medication
Narcotics
You will be given a prescription for a narcotic pain medication on the day of surgery. Take 1 – 2 tablets every 4 – 6 hours as needed for pain. These are given without refills.
If you need a refill, you must contact Dr. Carreira’s office, allowing 1 – 2 days to process, and this will be handled on a case-by-case basis.
Addiction to narcotics should not occur during the initial phase post operatively unless there has been a history of abuse prior to surgery or if the medication is taken unnecessarily. Please notify Dr. Carreira or his staff if you have a past history of substance abuse of any type.
Common side effects of narcotics are dizziness, drowsiness, nausea and constipation. If these symptoms or an allergic reaction (i.e. rash, hives, shortness of breath) occur, stop taking the medication and call Dr. Carreira’s office. To decrease possible side effects of the narcotics, make sure you take the medication with food.
Blood Thinners
You will be given 81mg of enteric coated aspirin twice per day after surgery for 3 weeks, unless you are at higher risk based on the blood clot assessment tool completed at your preoperative appointment. Patients who are determined to be at high risk of blood clots are provided a stronger blood thinner than aspirin.
Naproxen
Start the morning the day after surgery and take with food. You will take this medication two times daily for three weeks. THIS IS A SCHEDULED DOSE, NOT AS NEEDED. This will prevent excess bone (heterotopic ossification) from forming.
Omeprazole
Over the counter. Take with naproxen and blood thinners to prevent gut irritation or ulceration for at least 3 weeks after surgery.
Robaxin: (Methocarbamol) 750m
One pill every six hours as needed for muscle spasms.
Colace
Colace is an over-the-counter stool softener. Anesthesia and pain medication can cause constipation. Take daily until regular bowel movements occur. You should have a bowel movement no later than 2 days after surgery.
Anti-nausea
You will be given a prescription for Zofran, which is anti-nausea medications.
Antibiotics
You will not be given a prescription for antibiotic because you are given IV antibiotics prior to surgery.
Supplements
Multivitamin
- Nature Made ® Multi Complete Tablets are an excellent option, containing 180 mg Vitamin C, 2500 Vitamin A, and 1000 IU Vitamin D, as well as plenty of zinc, copper, and selenium.
- Centrum ® Men or Centrum ® Women is also a good option, with 90 mg (men)/70 mg (women) Vitamin C, 3500 IU Vitamin A, 1000 IU Vitamin D, and sufficient amounts of zinc, copper, and selenium.
Hydration
It is important to stay hydrated after surgery. It may be helpful to keep a bottle of water nearby and take frequent sips of water.
Dressing Changes
If the post-op dressing is soaked, you may remove the dressings and replace it with large gauze or abdominal (ABD) pad dressings during the first two days.
On day 3, you may remove the bulky dressing and xeraform (yellow stirps), then cover the sutures with Band-Aids. Use waterproof Band-Aids for showering and then replace with regular Band-Aids. In order to reduce risk of infection, please avoid touching your incision while replacing the bandages.
Keep your incisions covered with Band-Aids or dressings until 2 days after suture removal. Suture removal is planned for 3 weeks after surgery.
Pool therapy can be started without any coverage of the skin once there is full skin coverage without any breaks or scabs on the skin, typically 6 weeks after surgery. Avoid bathing, hot tubs, or whirlpool for 6 weeks after surgery.
Please avoid putting creams, Neosporin or oils onto the incision, including after suture removal. This may increase your risk of developing an infection.
Home Medications
Most home medications are safe to restart the day after surgery. If you have any questions about restarting your medications, please ask your primary care physician.
Driving and Flying
Legally, you are not allowed to operate heavy machinery, including cars, while taking narcotics. If surgery was performed on the right hip, be cautious about prolonged (greater than 10 minutes) driving in the first 4 weeks after surgery.
With regards to flying or longer traveling (greater than 2 hours) by car, precautions should be followed closely to prevent blood clots. During the time that you are not fully weight bearing, we recommend that you perform ankle pumps, which are repetitive motions of the feet up and down. If you are flying, we recommend getting up and using your crutches to move about approximately every hour.
Returning to Work or School
Returning to work or school depends on the type of surgery. For school or sedentary work, you may return within 1-2 weeks, as long as the pain is tolerable. However, you must take the time to honor your commitments to therapy and office visits, and you must follow all postoperative instructions carefully. Weight bearing status and special equipment may also affect your return to work/school date.
FMLA/Short Term Disability Paperwork
Peachtree Orthopedics has partnered with ShareCare to ensure the accurate and timely completion of your FMLA and/or disability forms.
https://peachtreeorthopedics.com/for-patients/
A detailed information packet regarding hip arthroscopy is provided for patients undergoing surgery. Many of the important details regarding the surgery and its recovery are reviewed to help guide patients during their recovery.
Sleeping
Sleeping in a prone position (on your belly) is recommended one to two hours per 24 hours to stretch out the hip flexors.
Arthritis and Hip Arthroscopy
This video demonstrates a 76-year-old man who is pain free just three weeks after hip arthroscopy.
This patient had no arthritis identified before surgery or at the time of surgery, which is unusual for a patient with hip pain at this age.
However, this case points out the fact that each patient individually needs to be assessed for arthritis regardless of age. Arthritis does occur more often as we age, but there are patients in their 30’s and 40’s who have severe arthritis and patients in their 60’s who have little to no arthritis.
The best imaging study to assess arthritis is a plain x-ray. If any joint space narrowing is noted, the arthritis oftentimes is too advanced for a hip arthroscopy procedure and a joint replacement or resurfacing is preferable.
Psoas Release After Hip Replacement
Following hip replacement surgery, further hip arthroscopy may be indicated in patients who have a painful psoas tendon following hip replacement surgery. The above video details the psoas release after hip replacement, with Dr. Carreira providing the voiceover for the video.
Placement of Suture Anchors During Hip Arthroscopy
In the short hip arthroscopy video below, Dr. Carreira demonstrates a view inside the hip joint of placement of a suture anchor. Following preparation of the rim of the acetabulum to a bleeding, bony surface, a cannula is then placed to allow passage of the necessary instruments for labral repair. A metal guide is placed first with spikes in it to help secure it to the bone during passage of the drill and anchor. A drill is passed to create space for the anchor. The anchor is then tapped into place using a hammer. The suture anchor is checked to confirm that it is securely in place. This check is done by pulling on the anchor. The sutures themselves are passed around the labral tissue.
Additional Hip Arthroscopy Videos
Dr. Dominic Carreira has posted additional videos on his YouTube channel.
American Association of Orthopedic Surgeons
The American Academy of Orthopedic Surgeons (AAOS) has an entire section of its website dedicated to providing detailed information about hip arthroscopy.
New Hip Arthroscopy Research Projects by Dr. Carreira and the Carreira Research Group
Dr. Carreira and the Carreira Research Group are currently conducting several clinical research studies regarding hip arthroscopy. Each study will focus on assessing and improving the current surgical standard of care. Patients that are candidates for hip arthroscopy are provided with the opportunity to contribute to the advancement of medicine. Qualifying candidates for the study may participate voluntarily by completing an informed consent process. For more information about this study, please contact Dr. Carreira.
The MASH Study Group
 The MASH Study Group is looking to find answers to difficult questions related to the surgical treatment of patients with adolescent and young adult hip injuries.
The MASH Study Group is looking to find answers to difficult questions related to the surgical treatment of patients with adolescent and young adult hip injuries.
Co-founded by Dr. Carreira, the Multicenter Arthroscopy Study of the Hip (MASH) Study Group is a group of fellowship-trained orthopaedic surgeons focused on the treatment of hip injuries and hip preservation in the athletic and pre-arthritic population.
More information about the MASH Study Group is available on its website, mashstudy.com.
Concierge Service for Out of Town Hip Arthroscopy Patients
Dr Carreira has created a concierge service for patients traveling from out of town. He has treated patients with hip injuries from various cities in the southeast, including Savannah, Augusta, and Macon, Georgia, Birmingham and Mobile Alabama, Asheville, and Charlotte, North Carolina; Columbia and Charleston, South Carolina; and Knoxville, Tennessee. Coordination of care will be provided after your visit when needed.